Baskin Clinic is committed to providing reliable support for our patients. We are here for you with any questions or symptoms you might be feeling. In the best interests of limiting contact, we’re going to be largely telehealth (voice, video, text, email) until conditions allow.
We are in the midst of a pandemic, well beyond the point of containment of the virus. We all must work to slow the spread (and the resultant surge in health care needs) so that health systems are not overwhelmed.
Please think of this page as a resource. We’ll be updating it regularly. Text in this color has been added or updated since April 7th.
If you are over 60, have chronic conditions, or have cold or flu symptoms, stay at home for the next 2 weeks (or more).
If you have cold or flu-like symptoms, behave as if you have COVID-19, and read the Treatment section below for additional guidelines.
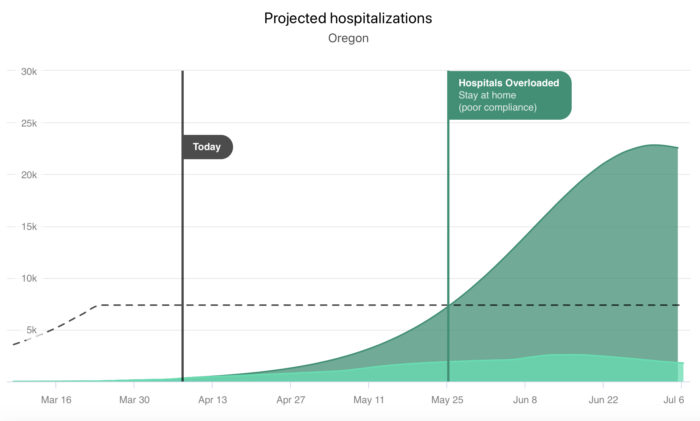
Are we flattening the curve yet?
The collective actions of Oregonians have enabled 140 life-saving ventilators to be shipped from here to New York. Oregon hospitals and ICUs are not overwhelmed. Social distancing has saved lives, and will continue to save many more in the weeks and months ahead. But social distancing must continue.
Multiple epidemiological models agree that by maintaining strict adherence to the current measures, Oregon will likely stave off the worst case scenarios we’ve seen play out in Italy and elsewhere. And unlike a weather forecast, we influence the disease models with our behavior right now, and tomorrow. We know there are many undetected cases in our community, and we have no idea how many. Some of the people who have the disease don’t realize they have it. We just heard from a colleague in Los Angeles — a pediatric surgeon on ER backup duty — who tested positive and has absolutely no symptoms whatsoever. None.
Relaxing our guard now could be catastrophic. We are still an overgrown forest in July, all dry tinder and little chance for rain.
As long as this disease exists in our community, there will continue to be outbreaks. As long as we keep our distance, these outbreaks will be mostly small. We can be hopeful, but we must be vigilant.
- Stay home.
- Wash your hands frequently.
- Don’t touch your face.
- And wear your mask in public places.
In the weeks to come, keep in mind that if you were to have the virus, the personal connections you are missing are the ones that you are protecting by staying away.
Stay home. Save lives.
In case you missed the details of Gov. Kate Brown’s orders, check out this graphic and click the link to view more information.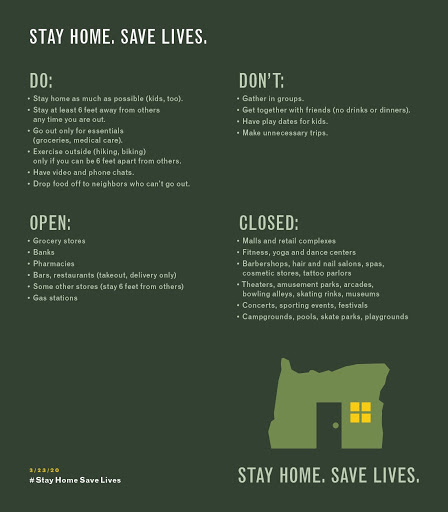 Additionally, on March 23rd, Gov. Jay Inslee announced even farther-reaching stay at home orders in the State of Washington. Before you venture out, please consider the restrictions that are in place and the potential impact of your actions at this critical moment.
Additionally, on March 23rd, Gov. Jay Inslee announced even farther-reaching stay at home orders in the State of Washington. Before you venture out, please consider the restrictions that are in place and the potential impact of your actions at this critical moment.
If I’m under 60, do I need to be concerned about getting COVID-19?
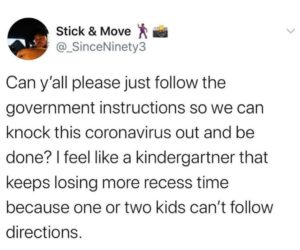
YES. Be a part of the solution, and not part of the problem. Asymptomatic carriers are just as hazardous to public health as symptomatic carriers. Plus, new data from the CDC shows that nearly 40% of patients hospitalized from COVID-19 have been between ages 20 to 54.
The less you practice social distancing, the greater your chances of infecting yourself or someone else. Even if your case isn’t severe, theirs may well be. The more quickly and strictly we practice social distance, the less impact the pandemic will have on our already-strained healthcare system.
Social Distancing Saves Lives

Social distancing is the best tool we have to slow the spread of COVID-19
New rules for congregating and socializing:
- Maintain distance — stay 6 feet away from other people. This includes work and non-work settings.
- Avoid crowds. In Oregon, gatherings of more than 25 people are banned.
- Protect at-risk groups, including: People over the age of 60, and people of any age with chronic health conditions like kidney or liver disease, heart or lung disease, diabetes, immunosuppression (chemotherapy or medications to treat autoimmune diseases like Crohn’s or rheumatoid arthritis), or pregnancy.
- Wash your hands. Handwashing and behavioral measures (keeping hands off the face) are effective ways to reduce transmission.
- Wear a mask. Combined with proper hand hygiene, a mask can help to reduce viral transmission.
- Assume common surfaces are potentially infected. The virus lives for up to 3 days on surfaces and is killed with household disinfectants (bleach, alcohol). See CDC Guidelines for what and how to clean.
- Cancel non-essential travel (both work and recreational), along with just about any group activity.
I feel great! Why would I need to isolate myself or participate in social distancing?

Without testing practices more widely in place, you have no way of knowing whether or not you are already infected. You could already be an asymptomatic carrier, or you may show symptoms later. Undetected cases of the virus were so prevalent in China, they are thought to be responsible for 86% of disease transmission. The fewer people you come into contact with, the slower the pandemic will spread. Slowing it down will help prevent hospitals from running out of rooms, doctors, and ventilators, allowing more people who need lifesaving care to access it, ultimately, saving lives.
Even people at lower risk for death, like younger people or those without chronic medical conditions, can still get infected, spread the coronavirus without having symptoms, or even get very sick and require hospitalization themselves. Right now, it is critically important for everyone to stay home as much as possible and stay at least 6 feet away from others when they must leave their home.
What should I do when I do have to leave the house?
Most of us are afraid of acquiring the coronavirus. One way to deal with this fear is to imagine that you do have the virus and change your behavior so you don’t give it to someone else. Pretend that anyone you see is your beloved but high-risk family member. Stay 6 feet away and try not to touch anything you don’t have to touch.
What precautions should people take while hiking/exercising outside at this time?
Continue to maintain a distance of 6 feet away from other people and pets while outside. Do not carpool with people outside of your household. Be extra prepared with water, snacks, sunscreen, your phone, and other emergency gear. Do not go into the backcountry or participate in activities that could result in injury or accident–emergency services are already overburdened right now. Try to explore new parks and greenspaces rather than the wilderness. Many trailheads, roads, and parks are closed at this time. Check before you go.
What about playdates for my kids?
Children are thought to be at low risk for serious illness due to COVID-19. However, it is believed they may be able to transmit the disease to others, even if not experiencing symptoms themselves. A small group of 1-2 friends might be okay for some family situations, but may be an unacceptable risk for families with closer connections to high-risk adults.
If you do arrange playdates, make sure the involved children have had no contact with sick individuals for two weeks, the groups involved do not have high-risk people in the household, and everyone washes their hands on arrival and frequently.
What about get-togethers with my extended family?
In all cases, more personal contact between groups of people increases the pathways along which the virus may be transmitted. Consider finding ways to “be together” other than in-person contact. We are discouraging larger groups getting together, especially since they usually include people in the at-risk categories (over age 60, or with chronic health problems).
What are the potential risks of food and grocery deliveries?
The main risk is if an infected delivery person coughs or sneezes on you since it is mostly transmitted from person-to-person contact.
However you could potentially contract COVID-19 from touching contaminated surfaces, then touching your face. There appears to be no risk from eating cooked food.
The safest option is to get your groceries delivered as you come into contact with the least amount of people.
When getting food delivered from a grocery store or restaurant, avoid close contact with the delivery driver; opt for the “no contact” option if available. Pay with a credit card. Throw away packaging and wash your hands before touching food. COVID-19 can live on cardboard for 24 hours and stainless steel and plastic for 2-3 days.
Remember the risk of infection from delivery is low, but unfortunately not zero.
How should I limit the spread of germs when ordering take out? Or going to the grocery store?
- Visit grocery stores or other unavoidable places at irregular times. Utilize curbside pickup options.
- Limit visit frequency by buying two-week supplies.
- While you’re in these places, do your best to give others personal space.
- Practice personal hygiene, with handwashing and avoiding touching your face.
- Wear a homemade mask, bandana, or similar covering for your mouth and nose.
You should have a 2-week supply of these items at home:
- Soap (not the antibacterial kind) for your hands, dishes, and laundry.
- Non-perishable foods like beans, rice, canned meats (chicken, tuna), frozen vegetables, and boxed/canned soups. Choose long-lived produce like apples and carrots.
- Prescribed medications to last several weeks.
- Paper towels and household disinfectant or make your own and put it in a spray bottle (1 tablespoon bleach in a quart of water, but you have to make it fresh each day). See CDC recommendations of what and how to clean
- Hand sanitizer: No Purell? You can buy a pump spray bottle and fill it with 70% rubbing (isopropyl) alcohol. Use lotion afterward.
- Thermometer, if you don’t already own one.
- Entertainment: games, magazines, books and e-books, videos, music.
- Over the counter medications. Consider acetaminophen (Tylenol) for fever and body aches, guaifenesin (Mucinex) to help loosen mucus and congestion, and dextromethorphan (DM, Delsym, Robitussin) to suppress cough if it is keeping you up at night.

Taking control over your risk of transmission
You’ve probably heard the terms droplets and aerosols a lot lately. Think of droplets like rain and aerosols like fog. When it’s raining you can put on a raincoat and open an umbrella to avoid getting your face wet. Raincoats and umbrellas aren’t so effective for keeping fog off your face.
Droplets are like rain
The good news is this virus spreads by droplets. The majority of COVID-19 cases are transmitted by droplets and not aerosols. So your greatest risk of transmission comes from (1) spending too much time in close proximity (less than 6 feet) to someone who has the virus, or (2) touching your face with a contaminated hand.
People touch their faces all the time, an average of 9-26 times per hour. Chances are good that you’ve touched your face at least once since you started reading this. The virus survives on surfaces, waiting for a hand to come by and deliver it to the mouth, eyes, or nose. The more surfaces you touch, the more opportunities you have to deliver the virus to your face.
When you are out in public, it is imperative that you not touch your face with a potentially contaminated hand.
To reduce the likelihood of accidentally touching your face with a contaminated hand, we recommend:
- Bring a little hand sanitizer bottle, or rubbing alcohol spray, with you to disinfect your hands after touching things.
- Wash your hands before you leave home and when you return home.
- Disinfect things you may have touched in-between, like your keys or phone. (It’s a good idea to clean your phone several times a day. Use an alcohol wipe or 70% rubbing alcohol spray.)
- Wear a mask while in public.

We recommend that people wear a mask while in public settings.
Yes, medical masks are in short supply and should be reserved for front-line personnel. However, multiple studies have demonstrated that non-medical masks (scarf, bandana, cloth masks, or something home-stitched) can be effective in reducing viral transmission. Instructions for sewing a mask may be found here. Also, wearing a mask can help you to not touch your face. This especially applies to those who still work at jobs in the community, are in a high-risk population, or care for others who are ill.
A mask is only beneficial when used in conjunction with proper hand hygiene and social distancing behaviors. Clean your hands before applying and after removing your mask. Clean your mask frequently by boiling it or washing in the washing machine.
Aerosols are like fog
Lastly, while aerosol transmission of the virus appears to be uncommon, there is still a possibility of this mode of transmission.
If you use a nighttime CPAP, or a nebulizer, these generate respiratory aerosols. There is also suspicion that dozens of people at a Washington-area choir practice were infected by aerosolized virus. For this reason, it is important to limit exposure to possible aerosols.
- Limit your exposure by following the governor’s stay at home orders.
- If someone in your household becomes ill AND uses CPAP or a nebulizer, it may increase the chance of spreading the virus within your household. Take extra care to isolate in these situations.
When should I wear a mask?
Please keep in mind that a mask is not a substitute for hand hygiene, proper distancing, or limiting trips outside the home. As a general rule, you should consider wearing a mask any time you are likely to be within 6 feet of another person who isn’t a member of your household. This is most important with indoor settings where potential aerosols may linger. However, if you were to cough upwind from another person at the dog park,, I bet that person would appreciate you wearing a mask.
How should I wear a mask?
Make sure your mask fits snugly around your mouth and nose, and is secure enough that you won’t have to fiddle with it while you’re out in the world. Once the mask goes on, DO NOT TOUCH it until it’s time to remove it. Remember, it’s filtering the air you breathe, and may be trapping coronavirus and other germs.
When it’s time to remove the mask, first wash or sanitize your hands. Then carefully remove the mask from behind your head/ears. For washable masks, place it directly in the washing machine and wash before reusing it. For disposable masks, you can place your mask in a paper bag for at least three days, then reuse it.
After removing your mask, youur hands may be contaminated with coronavirus. Wash your hands, and disinfect any surfaces you may have touched.
What mask should I use?
The CDC has provided a nice resource for making masks at home, with or without sewing required. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html
Mental Health During the Pandemic
Our mental health partners, Drs. Michael Leidecker and Michelle Bobowick at Clearwater Associates, have provided these suggestions for emotional self-care:
Limit (not end) the intake of news. We recommend relying, at the most, on one or two trustworthy sources of information and checking them no more than twice a day.
Stay connected. Isolation feeds anxiety, so rather than texting family and friends, we promote picking up the phone or video chatting with loved ones directly.
Take care of your body. Engage in physical exercise and healthy nutrition. Take deep breaths, stretch, or meditate. Prioritize healthy nutrition choices and well-balanced meals. Get plenty of sleep and limit alcohol and drugs.
Have a sense of purpose. Offer to walk a neighbor’s dog when they are more compromised during this time. Make multiple extra meals and offer to leave on neighbors’ porches. Investigate ways to volunteer safely in the community.

Symptoms
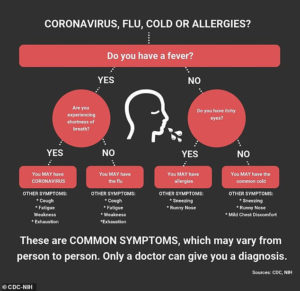
 The most common symptoms of COVID-19 are fever, fatigue, and dry cough. People with fever, cough, and difficulty breathing should seek medical attention.
The most common symptoms of COVID-19 are fever, fatigue, and dry cough. People with fever, cough, and difficulty breathing should seek medical attention.
- Runny nose is much more likely to be a cold or seasonal allergies.
- Stomach symptoms without fever, like diarrhea, nausea, or vomiting are much more likely to be viral gastroenteritis (also known as a stomach bug).
- Loss of senses of smell and taste have been reported as early symptoms, often presenting before the onset of other symptoms.
Some people become infected but don’t develop any symptoms and don’t feel unwell. Most people (about 80%) recover from the disease without needing special treatment.
Around 1 out of every 6 people who gets COVID-19 becomes seriously ill and develops difficulty breathing. Currently, 38% of US cases that require hospitalization are between ages 20-54. Older people, and those with underlying medical problems like chronic lung disease, heart disease or diabetes, are more likely to develop serious illness.
Testing
Testing availability continues to increase. As of 4/6/20, there have been 21,801 lab tests for COVID-19, and 1,132 confirmed cases of the disease in Oregon. Regardless of the capacity increases, the Oregon Health Authority continues to recommend that people only seek a test if they need to interact with healthcare personnel. In other words, unless you are sick enough to require medical evaluation (or if you are a healthcare provider yourself), you will not qualify for a test. Instead, exercise self care and isolate yourself within your home until 72 hours after you are free of symptoms. If you are experiencing symptoms consistent with COVID-19, please inform your Baskin Clinic physician.
By avoiding unnecessary tests, we reduce the risk of transmission within our healthcare system, AND we conserve precious clinical resources.
What about testing to see if I have had COVID-19 already?
Scientists are working to develop a serological test — one that can detect antibodies in people who have recovered from COVID-19. The data regarding the risk of reinfection for those who have recovered from COVID-19 is also unclear. At this time, it is best to continue focusing on social distancing and reducing pathways for spreading the virus.
Treatment
If you or a member of your family gets sick, others in your family are more likely to get it too.
Your goals are now to slow the spread of the virus in the house, care for one another, and prevent the virus from leaving your home.
- If you or someone in your household is sick, that person should stay home except for medical visits.
- Others in the house should not leave the house, if at all possible. Exercise utmost care if you must leave the house.
- Do not allow anyone else to enter the home.
- Use delivery services for food and other household necessities.
- As much as possible, the sick person should self-contain in a separate room (and separate bathroom) from other household members.
- Disinfect all high-touch surfaces daily.
- Do not share household items.
- Pets should be treated like impossible-to-clean, frequently-touched surfaces. Your pets probably won’t get the virus, but are likely to carry it to others who touch them. People should wash their hands before and after interacting with pets.
- Infected persons should wear a facemask when around other people or pets. If they cannot obtain a mask, use a bandanna, shirt, or other layers of cloth to cover the nose and mouth when leaving their separate room. If they cannot wear a mask, then others should wear one when interacting with them.
- Monitor symptoms, and contact us if things are getting worse.
I feel better. When can I go back to following normal social distancing guidelines?
- You have had no fever for at least 72 hours (that is three full days of no fever without the use medicine that reduces fevers)
AND - other symptoms have improved (for example, when your cough or shortness of breath have improved)
AND - at least 7 days have passed since your symptoms first appeared
I have heard (chloroquine, heat therapy, zinc, etc.) are effective treatments for COVID-19. Can you order for me?
Rest assured, your Baskin Clinic doctors are staying abreast of best practices in COVID-19 treatment. Currently, there are no controlled or validated data for the use of any novel therapy or medication. We will continue to closely monitor the medical literature
The FDA has been working closely with other government agencies and academic centers that are investigating the use of the drug chloroquine, which is already approved for treating malaria, lupus and rheumatoid arthritis, to determine whether it can be used to treat patients with mild-to-moderate COVID-19 to potentially reduce the duration of symptoms, as well as viral shedding, which can help prevent the spread of disease. Studies are underway to determine the efficacy in using chloroquine to treat COVID-19.
The Oregon Board of Pharmacy has issued an emergency rule preventing pharmacies for filling prescriptions for chloroquine and hydroxychloroquine to patients in outpatient settings unless they have a diagnosis of rheumatoid arthritis or other approved uses.
I heard that ibuprofen and other NSAIDs can make the disease worse. Is that true?
We’ve heard that rumor too, and it is purely theoretical, with no clinical data to substantiate it. That said, for a mild fever, we recommend taking nothing and letting your body’s natural immune response do its work. If the fever goes over 103 or if you’re feeling too uncomfortable with body aches and such, acetaminophen is a safe choice for most people.
Frequently Asked Questions
What chronic conditions have been linked to increased COVID-19 risks?
Chronic lung disease
Moderate or severe asthma
People who are immunocompromised
Severe obesity (BMI >40)
Diabetes
Kidney failure
Liver disease
Pregnancy is a potential risk for infection, but has not been shown to increase risk.
Many conditions can cause a person to be immunocompromised, including cancer treatment, smoking, bone marrow or organ transplantation, immune deficiencies, poorly controlled HIV or AIDS, and prolonged use of corticosteroids and other immune weakening medications
https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/people-at-higher-risk.html
If I’m in the high-risk population, what can I do to decrease my risk of serious illness?
- Strictly adhere to social distancing and personal hygiene recommendations.
- If you smoke or vape, quit right now. Contact your doctor and connect with 1-800-QUIT-NOW for support.
- Do your best to control any chronic medical conditions, such as keeping your blood sugar and blood pressure at goal levels.
- Practice self-care, including adequate sleep, moderate exercise, a healthful diet, and reducing stress levels when possible.
I have asthma, what should I do?
Presently, all indications are that you can stay on your current medications. There is no need to change to a nebulizer if you were to get COVID-19. Additionally, the American College of Allergy, Asthma and Immunology is encouraging patients to stay on their inhalers and nasal steroid sprays for allergies if needed.
I heard that certain blood types are more at risk. What’s up with that?
This is not something that should be shaping your behavior at this time. An initial study that has yet to be peer reviewed for publication has identified the possibility that blood type may be associated with hospitalization due to COVID-19. However, the link is not strong enough to present a clear case and does not provide evidence of causation.
All people should take precautions (handwashing, social distance, etc.) to reduce their risk of acquiring or transmitting the virus.
If you feel comfortable with taking a small risk to help the nation, there is an urgent need for blood donations.
I heard that if my blood pressure medication is an ACE inhibitor or an Angiotensin Receptor Blocker (ARB) it may increase my risk for COVID-19 and/or the severity of the disease. Is that true?
Right now, it is best to continue using your medication as prescribed. The American College of Cardiology, American Heart Association, and Heart Failure Society of America have stated that there is currently no evidence that ACE inhibitors or ARB medications affect outcomes for people infected with COVID-19. Read their statement here. Additionally, uncontrolled high blood pressure is known to increase risk of death from all causes, including COVID-19. Please stick with your usual treatment plan.
The pharmacy says it has not received your fax for my prescription refill. Can you resend it?
Pharmacies are running behind in processing faxes at this time. Rest assured, our medical assistants have faxed your prescription, and the pharmacy does have it, even if they don’t know it yet. Please anticipate delays in the pharmacies processing refill requests.
How long does the virus survive on surfaces?
Early study results from the National Institutes of Health, Princeton and UCLA indicate that COVID-19 may be viable for up to 4 hours on copper, up to 24 hours on cardboard, and up to 2-3 days on plastic and stainless steel.
What disinfecting products work on COVID-19?
The EPA has released a list of 200 disinfectants that are approved for use on COVID-19. Common active ingredients to look for include: sodium hyperchlorite, quaternary ammonium, hydrogen peroxide, ethanol, thymol (natural, thyme derived), and glycolic acid. Do not mix different disinfectants together, as this can create poisonous chemicals.
Is Baskin Clinic open for other health concerns?
In the best interest of keeping our patients and staff safe and healthy during this time, we are encouraging all patients to use our telehealth options. For issues that simply must be resolved in person, please talk with your doctor to arrange care.
What is the best way to reach my Baskin Clinic doctor?
Phone, text, and video chat with your doctor using the Spruce platform. Email is also good.