Just like it’s important to assess your exposure risks and act accordingly, it’s important to understand the limits and best practices around testing for the virus, which has made a comeback. Two weeks ago, we discussed how the State of Oregon could have a new record of 312 cases soon, and that number was surpassed within two days. Yesterday, we had a record 437 cases. The forecast model used by the Oregon Health Authority suggests a viral reproduction rate of 1.4, which would put us on track for over a thousand daily cases in the coming weeks.
We must do everything we can to reduce the transmission now, which of course extends to the testing process.
The Problem with Using Testing as a Shortcut:
A person can get exposed on Sunday.
Get tested Monday.
Get a negative result Wednesday.
Attend a meeting Thursday.
Start feeling symptoms Friday (“but I was negative”).
Get tested Saturday.
Only to be positive on Monday.
Did they spread the virus to coworkers, family, or friends on Thursday?
Bottom line: a negative test is no guarantee. It merely shows whether the person had enough of the virus at the time of testing to cause a positive result. And even then, the viral test misses positive cases about 30 percent of the time. We must rely on good choices and behaviors, not testing, to reduce the spread.
Sidenote: The State of Oregon is now expecting capacity to decline over the next 6-8 weeks because of the strain on supply lines from the national surge in cases. There was a 29% drop in tests performed in Oregon over the week of July 6-12.
Who Can Get Tested?
Those with symptoms can get tested.
Those without symptoms, but have had a high-risk exposure (defined as 15 minutes within 6 feet of a known positive case) can get tested. Additionally, those in a vulnerable group, including those who:
- live or work in group settings,
- are black, indigenous or other person of color,
- have a disability,
- are not native English speakers.
Travel During the Pandemic:
All travel is discouraged. If travel seems necessary, choose travel that doesn’t include close contact with other people, like road trips, camping, or renting a house or private Airbnb. Definitely avoid resorts, cruise ships, bars, and indoor restaurants.
In a recent Washington Post article, Dr. Fauci and other experts were asked about their personal behaviors with regard to travel, eating out, and other activities.
Our takeaway — Dr. Fauci’s own daughter didn’t just take a test and call it safe when she came to live with him. She did a 14-day quarantine before giving him a hug. Testing is not a pass for non-emergency travel because traveling itself is high risk. For those who do travel, plan to self-isolate upon arrival, and again after returning home.
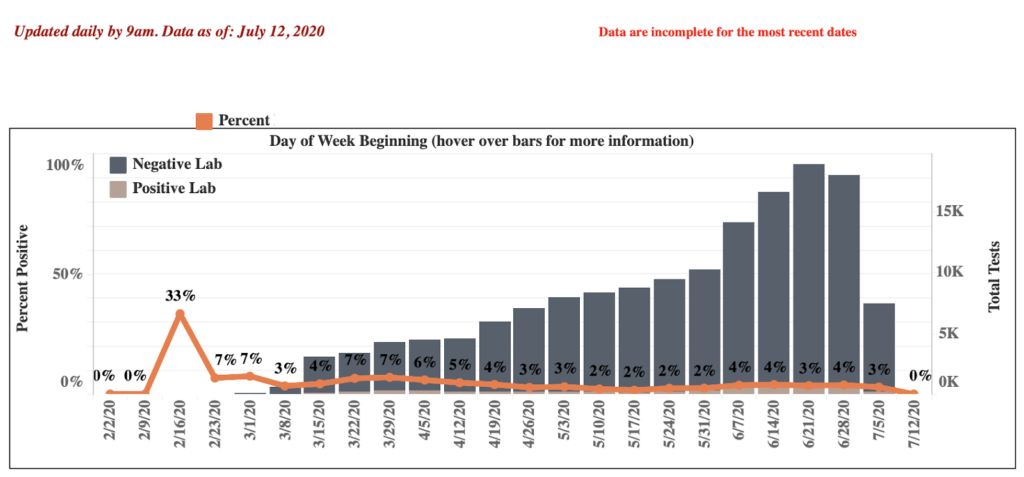
How Do We Know the Increased Case Counts Aren’t Just Due to More Testing?
Some of the increase in absolute numbers of cases is due to increased testing, but this is an insufficient explanation. While the number of tests per day doubled from May to June, so did the percent of those tests coming back positive. So we would have to re-double our testing capacity if we wanted to compare apples.
Additionally, contact tracers are now following up on nearly all positive cases within 24 hours, but they are finding that about 40 percent of new positive cases are not linked to other known cases. This has also been trending upward since May. This suggests that community spread rather than clustered outbreaks or superspreader events is driving the increasing positive test rate in the Metro area. The qualifications for testing today are less strict than they were in May, casting a wide net, rather than focused on relatively high-probability patients.
Since we would have to re-double the testing we’re doing now to achieve the same positive test rate that we had in May, the positive cases we find are less likely to be traced to other positive cases, and the rules for testing allow for testing in lower probability situations, we don’t have a good reason to believe that testing is simply capturing a larger proportion of the cases in the community.
What Do We Make of Lower Hospitalization and Death Rates?
Hospitalizations and death rates are important metrics to gauge the severity of a disease, and its impact on our healthcare system. With COVID-19, rates could be declining for a number of reasons. Most significantly, we are now seeing a greater proportion of our positive cases in young people, who typically experience less severe disease. Among Metro-area residents in their 20s, only 3.1 percent of positive cases have been hospitalized, and 0 have died. For positive cases of people in their 60s, 29.6 percent have been hospitalized, and 27 have died. So the declining hospitalization rate could be because more young people are getting the disease.
It could also be that more accessible testing simply is finding more people who have no symptoms or mild symptoms, which would also explain the increase in young people.
More mild cases of the disease wouldn’t necessarily be a problem if the infected people could somehow avoid giving it to more vulnerable people. But that’s unlikely to happen.
We should also note that some of the decline in death rate may be because doctors are getting better at treating COVID-19. And some of the declining death rate may be related to people getting lower amounts of the virus because of masks, social distance, or other reasons.
On a Lighter Note
As you know, we’d always like to end with something fun. If you’re staying home instead of going to visit our National Parks this summer, these posters made from 1-star yelp reviews may help you realize you’re not missing anything.
And if you yet haven’t done so, please take 3 minutes to share your feedback about the Baskin Clinic pandemic response.
Take care,
Baskin Clinic